Typhoidal Salmonella
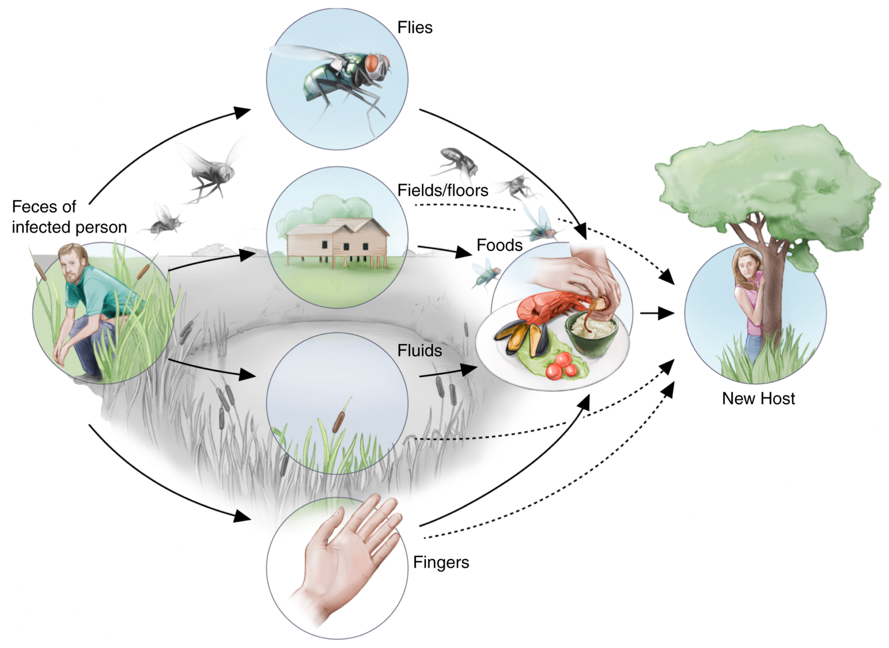
Salmonella enterica serotypes Typhi, Sendai, and Paratyphi A, B, or C are found exclusively in humans. These serotypes, collectively referred to as typhoidal Salmonella, cause enteric fever (also known as typhoid or paratyphoid fever if caused by serotypes Typhi or Paratyphi, respectively). Most often, enteric fever is acquired through ingestion of food or water contaminated with human feces. Typhoid fever is an invasive, life-threatening systemic disease with an estimated global annual burden of over 27 million cases, resulting in more than 200,000 deaths. It is endemic in developing countries particularly in the Indian subcontinent, South and Central America, and Africa. These regions share several characteristics such as rapid population growth, inadequate human waste treatment, and limited safe water supply, which may contribute to the spread of disease.
Typhoid fever is uncommon in the United States. About 350 people are diagnosed with typhoid fever, and 90 people are diagnosed with paratyphoid fever each year in the U.S. These case numbers do not include people who do not seek medical care, who are not tested for either typhoid or paratyphoid fever, or whose disease is not reported to the Centers for Disease Control and Prevention (CDC). Taking into account these unreported cases, CDC estimates that typhoid fever affects 5,700 people in the United States each year. The CDC has not made estimates for the annual number of cases of Salmonella Paratyphi. In 2015, there were 309 typhoid fever cases reported to the CDC by 38 health jurisdictions. Twenty-four health jurisdictions reported 71 paratyphoid fever cases, all of which were caused by Salmonella serotype Paratyphi A.
Most U.S. residents who are diagnosed with typhoidal Salmonella are infected while traveling abroad in areas where typhoid fever and paratyphoid fever are common. Three types of vaccines against S. Typhi are commercially available, although there is still not a single licensed vaccine available against S. Paratyphi A. Persons planning to travel outside of the United States are advised to find out if a vaccine for typhoid fever is recommended (see www.cdc.gov/travel).
Nontyphoidal Salmonella
In contrast to typhoid fever, which is common in developing countries but not in developed nations, nontyphoidal salmonellosis occurs worldwide. Salmonella infection is recognized as a considerable burden of illness in both developing and developed countries. Globally, there are an estimated 93.8 million cases annually of gastroenteritis due to nontyphoidal Salmonella serotypes, resulting in approximately 155,000 deaths.
Salmonellosis is a nationally notifiable disease in the United States. Reports of Salmonella infections acquired from any source (water, food, environmental exposure, etc.) are made to the CDC via a passive, laboratory-based surveillance system conducted in 50 states and the District of Columbia. During 1996-2011, a total of 608,571 Salmonella isolates from humans were reported to the CDC. The overall average for the 16-year period ranging from 2004 to 2011 was 14 cases per 100,000 persons. The number of cases per 100,000 persons has stayed relatively steady since then.
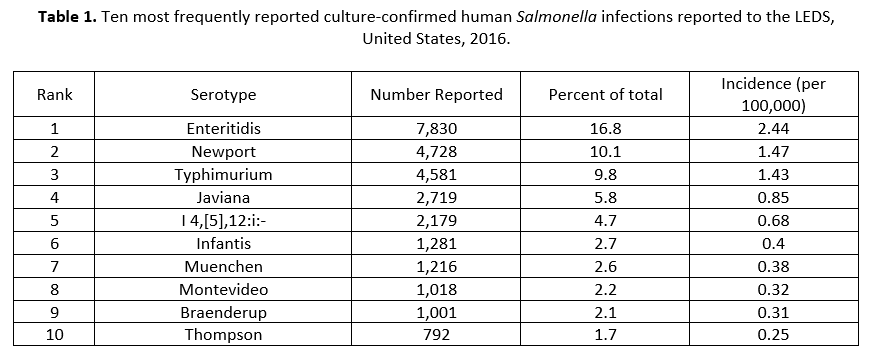
In 2016, 53 state and regional public health laboratories reported 46,623 cases of culture-confirmed Salmonella infections to the CDC Laboratory-based Enteric Disease Surveillance (LEDS) system with an average of 14.51 cases per 100,000 population. Table 1 shows the ten most reported serotypes in the United States in 2016.
As in previous years, the largest percentage of cases in 2016 were reported in the summer months. Infants (children <1 year old) had the highest incidence of infection (110.81 cases per 100,000 population for boys and 108.81 for girls) (see Table 2).

There are no vaccines against nontyphoidal Salmonella available for use in humans. There are effective vaccines for use in poultry, but none is available for use in other animal reservoirs such as cattle or pigs. This represents a significant limitation in existing prevention strategies.